Chin-Hsien Lin, Department of Neurology, National Taiwan University Hospital
Parkinson's disease (PD) is a prevalent neurodegenerative disorder characterized by the aggregation of alpha-synuclein proteins in dopamine neurons within the brain, leading to dopaminergic neuronal degeneration. Current available treatments for PD only provide symptomatic relief, and mechanism-targeted therapy to mitigate the disase progression is still lacking. Identifying the pathogenic genes for hereditary PD helps unravel the molecular mechanisms underlying the disease and facilitates the development of novel drugs.
In our previous research, we established fruit fly and mouse models carrying the PD-associated LRRK2 G2019S gene mutation. Our investigation into how the LRRK2 mutation activates GSK3β kinase revealed mechanisms leading to increased tau phosphorylation and neuronal apoptosis (J Neurosci, 2010). Using this as an FDA-Approved Drug Library platform, we discovered that by activating the Akt/NRF2 pathway, lovastatin has neuroprotective effects to slow down dopaminergic neurodegeneraition (Hum Mol Genetics, 2016; Mov Disord, 2021). Additionally, we successfully corrected this mutation in the patient-derived iPSCs using gene editing techniques (Stem Cell Res Ther. 2021). Our team also constructed Asia's first comprehensive genetic blueprint for young-onset and familial PD (Mov Disord, 2019) and identified UQCRC1, a novel PD-causative gene for familial parkinsonism combined with polyneuropathy (Brain, 2020; Cell Rep, 2021). In addition to genetic factors, changes in the gut microenvironment through the gut-brain axis are considered one of the triggers for PD. The interaction between genes and the gut microenvironment is currently a research topic of utmost importance (Figure 1).
With the maturation of technologies in gene and nucleic-acid-based therapeutics—such as the recent FDA-approved gene therapy for spinal muscular atrophy, a disorder caused by a deficiency of the SMN1 gene—we have witnessed a successful instance of gene therapy extending beyond laboratory research and into clinical settings. Several new technologies are emerging as potential avenues to slow the progression of neurodegenerative diseases. These include RNA-based nucleic acid therapy combined with viral or non-viral delivery system to specific brain regions, and even CRISPR/Cas9-based gene editing for specific mutations of disease-causing genes (Figure 2). Meanwhile, the development of biomarkers rooted in the mechanisms underlying the disease will assist future biotyping patient populations for individual mechanism-oriented therapy. In the future, precision medicine will proceed in this direction and pave a way to treat neurodegenerative diseases.
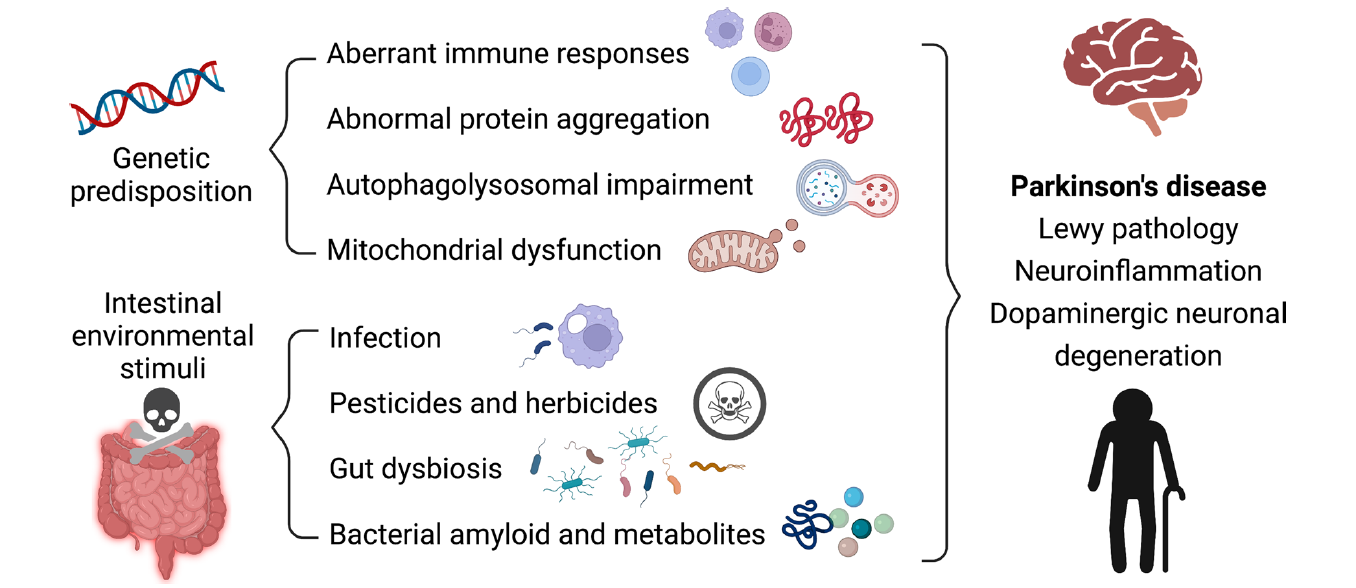 Figure 1: Through different molecular mechanisms, the interactions between host genetic variations and the gut microenvironment all lead to the same outcome: an imbalance in the regulation of alpha-synuclein protein, causing degeneration of predominately-dopaminergic cells (Figure from Chen SJ and Lin CH. J Biomed Sci. 2022 Jul 27; 29(1):54.).
Figure 1: Through different molecular mechanisms, the interactions between host genetic variations and the gut microenvironment all lead to the same outcome: an imbalance in the regulation of alpha-synuclein protein, causing degeneration of predominately-dopaminergic cells (Figure from Chen SJ and Lin CH. J Biomed Sci. 2022 Jul 27; 29(1):54.).
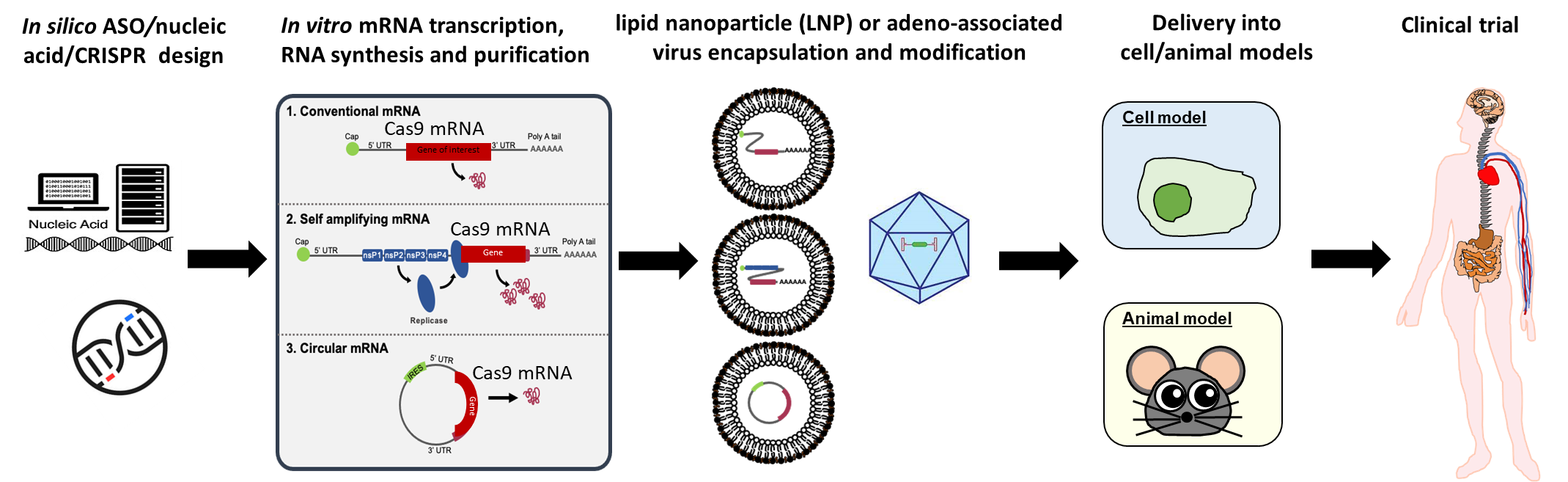 Figure 2:
Figure 2: Gene segments or nucleic acid drugs are delivered into targeted cells using virus or non-virus lipid nanoparticles to slow the transcription or translation of disease-related proteins and reduce the accumulation of disease-specific proteins in cells, thereby slowing disease progression and neurodegeneration.